The idiopathic epiretinal membrane (ERM) is a semitranslucent, glial, fibrocellular membrane that forms on the inner surface of the internal limiting membrane (ILM) at the macula. It is present in as many as 35% of adults over age 65 without any pre-existing comorbid retinopathy.1 It has been studied extensively, both in its epidemiological aspects and pathophysiologic mechanisms. The first documented surgery to remove an ERM was performed by Machemer in 1978.2 And, although many questions remain as to its causation, understanding outcomes has been a larger subject.
As the number of intraocular surgeries (per 1,000 individuals) increases—advancements in surgical technology allow for surgery in cases for which ERM was previously not indicated—so too do the concerns over surgical outcomes.3 As many as 10% of all vitrectomy surgeries performed in the United Kingdom are for an ERM indication (Figure 1).4 Results vary from patient to patient, so it remains a challenge to set universal post-treatment visual expectations for patients in confounder-free cases where refraction and media have been adequately addressed.
Cohort studies have shown that visual function and retinal anatomy improve with surgical removal (Figure 1).5,6 However, the timing of the surgery is an important element. Nearly a quarter will regress over time, but for the majority of patients, their condition either remains unchanged or worsens.7
The way in which ERM influences visual function and how those functional and clinical features tend to predict surgical outcomes has also been widely studied. Prior to the advent of optical coherence tomography (OCT), researchers found that if visual function was worse, the magnitude of improvement was greater after surgery.8 Yet, Snellen acuity and assessing a patient’s Amsler grid are merely part of the whole in today’s clinical setting. Knowing various anatomic features of the patient’s retina may play an important role in predicting outcomes, and has been the subject of some study since the widespread use of OCT.
OUTER RETINAL CHARACTERISTICS
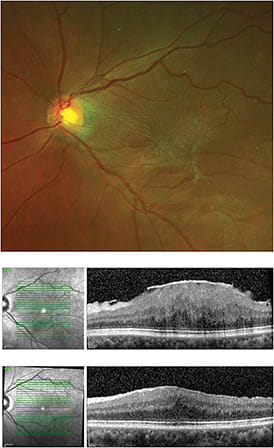
Some of the first forays into using OCT as an attempt to predict outcomes came in the form of evaluating the outer retina. In a 2012 study, Kim and colleagues found that if the inner segment/outer segment (IS/OS) was not readily identifiable or disrupted prior to surgery, mean final best-corrected visual acuity (BCVA) was 0.64 (logMAR, approximately 20/100 Snellen) in the disrupted group and 0.07 (logMAR, approximately 20/20 Snellen) in the intact group 12 months after surgery (accounting for media opacity and refractive error).9 Figure 2 demonstrates such an example.
However, the magnitude of visual gain in each respective group was not different, although the final results differed.9 Similar findings were replicated by Shimozono et al., who made further attempts using spectral-domain OCT to discern any differences when evaluating those with an intact IS/OS but attenuated cone outer segment tips (COST).10
They found that patients experienced earlier gains when IS/OS and COST were intact, as compared with intact IS/OS but attenuated COST. However, this difference was not present by 6 months. Ultimately, they found IS/OS was the dependent variable, reproducing the work of Kim et al.9,10
Because Shimozono could not find enough enrollees to determine whether external limiting membrane (ELM) attenuation was a dependent variable, Watanabe and others presented an analysis in which ELM was included, showing that COST derangement was an important longitudinal variable in addition to IS/OS and ELM.11 Those patients evaluated by Watanabe did not undergo surgery, therefore one cannot predict these findings’ contribution to surgical outcomes in a post hoc analysis. Some consider this finding predictive, but in the absence of direct comparison, knowing the ELM’s independent contribution may be only inferred.
Based on the above work, it appears that to the extent that the inner and outer segments, cone outer segments, and ELM are affected by an ERM, the worse acuity will be over time, and may predict worse acuity outcomes.
MACULAR THICKENING
In addition to IS/OS and COST changes, overall macular thickening has been identified as a potential predictor of worse outcomes, whether or not enervation to IS/OS or COST are found. In a review in which 101 eyes underwent surgery, the average presurgical thickness was 426 um and was reduced to 321 um.12 There was a significant improvement in BCVA and metamorphopsia over the 6 month postoperative period only in those eyes in which the macula was relatively thick and there was no identified loss of IS/OS on OCT. Authors found macular thickness was supplanted in its predictive value by implied injury to the IS/OS.
Seeming to contradict this finding, Massin and colleagues published a study of 62 eyes with 22-month average follow-up stating that average macular thickness did not correlate well with outcomes.13 This was published in 2000, prior to the advent of spectral-domain OCT, and most patients were evaluated using low-resolution B scan images. For example, the authors stated that it was difficult to find an ERM because the growth “was seen in only 42% of cases,” and more visible when the membrane was “slightly separated from the underlying retina” and that “it was difficult to differentiate…from the normal backscattering of the optic nerve fiber layer.”13 However, as OCT technology has advanced significantly through the years, this experience was later contradicted by a 1996 study showing a different relationship that has been reproduced.14-16
Macular thickness may be another factor in determining outcomes. It may be that the thicker the overall macula is, the worse the outcome in surgery.
ECTOPIC INNER FOVEAL LAYER
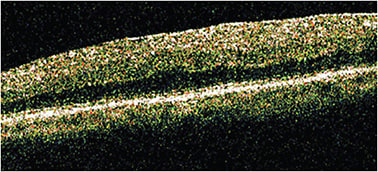
As the study of ERM has evolved, other features within the middle retina have been identified as potential predictors of outcomes, namely an ectopic inner foveal layer. Govetto and colleagues noted that in the more progressed stages, in which other elements, such as thickening and IS/OS attenuation, may or may not occur, layers within the retina showed communication independently.17 They found that the inner nuclear layer (INL) and inner plexiform layer (IPL) in particular seemed to demonstrate mobility or invasion into other inner retinal compartments where they are not normally found (Figure 3). Govetto et al. constructed a grading scheme, while accounting for outer retinal changes previously noted.17
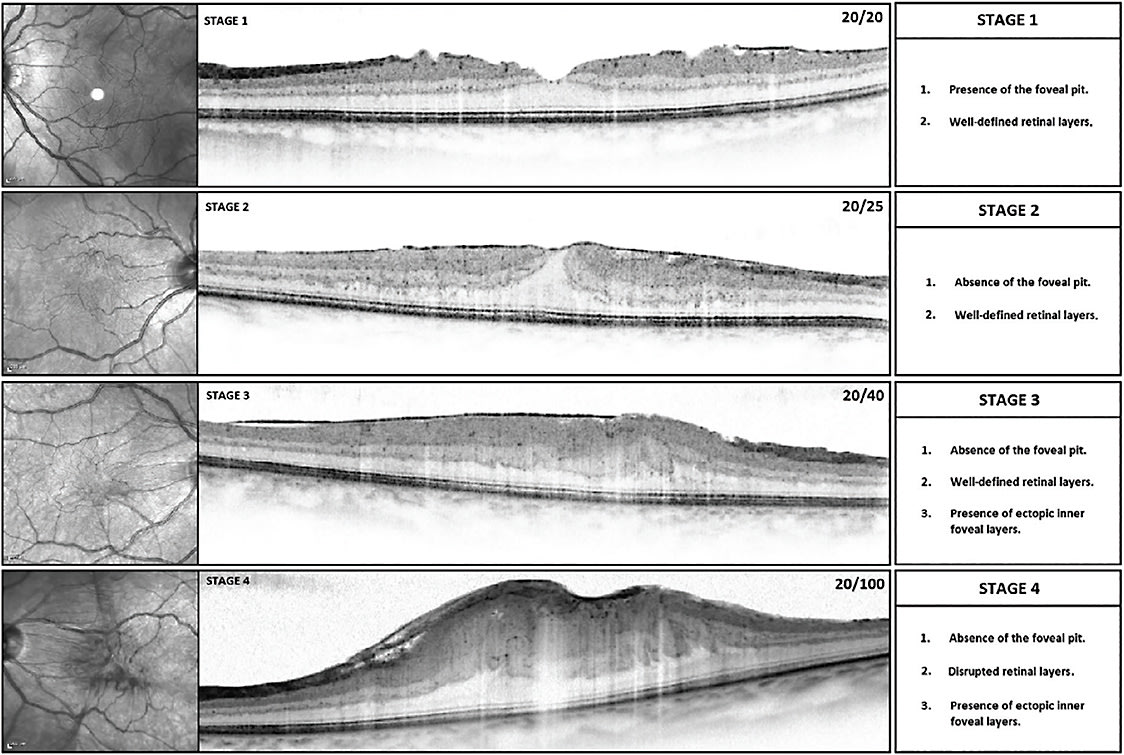
In this scheme, Stage 1 is when the macula shows the presence of an ERM, yet the normal retinal layers are discrete—particularly that the outer nuclear layer (ONL) spans the central fovea. As stages progressed, the INL and IPL mobilized centrally, covering the ONL. This was described as ectopic, given that only the ONL is normally present over the fovea, with the INL and IPL tapering and eventually becoming absent over the umbo. By Stage 3, the layers of the retina are distinct, but the INL and IPL have covered the ONL and umbo. Stage 4 occurs when there is an ectopic INL and IPL, and layers are no longer distinct.
Using this system, the authors found that the further a patient progressed—even identifying that IS/OS and COST were intact and the foveal avascular zone showed preserved perfusion—vision was degraded. The authors felt that an ectopic inner foveal layer, based on multivariate linear regression, was an independent risk factor for vision loss. One unfortunate feature of this work is that there was no pre- or postsurgical analysis. Therefore, we await post hoc correlation.
In short, aside from outer layer interruption and overall thickening, middle retinal characteristics may be predictive for surgical outcomes. Similar to some studies describing ELM contribution, this is merely theoretical until a well-designed intention to treat study can be conducted with perioperative comparisons.
CONCLUSION
Since the advent of OCT, anatomic features have been studied in ERM and have been found to be useful in predicting surgical outcomes in several instances. History, physical exam findings, and measured acuity still serve as the foundation in the overall assessment of predicted outcomes, but more clarity in the form of anatomic studies have added to predictive capabilities.
Particular elements of the internal anatomy of the macula, including IS/OS, COST, and ELM attenuation, overall thickening, and the presence of an ectopic inner foveal layer, have been shown to either correlate with worse acuity or worse predicted surgical outcomes (Table 1). Still, much work is needed to understand the pre- and postsurgical outcomes. NRP
| WORSE VISION | WORSE SURGICAL OUTCOME | |
| IS/OS attenuation | X | X |
| COST attenuation | X | X |
| ELM attenuation | X | |
| Thickening | X | X |
| Ectopic inner foveal layer | X |
REFERENCES
- Klein R, Klein BE, Wang Q, Moss SE. The epidemiology of epiretinal membranes. Trans Am Ophthalmol Soc. 1994;92:403-430.
- Machemer R. [The surgical removal of epiretinal macular membranes (macular puckers) (author’s transl)]. Klin Monbl Augenheilkd. 1978; 173(1): 36–42.
- Wubben TJ, Talwar N, Blachley TS, Gardner TW, Johnson MW, Lee PP, Stein JD. Rates of vitrectomy among enrollees in a united states managed care network, 2001-2012. Ophthalmology. 2016;123(3):590-598.
- Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL. United Kingdom national ophthalmology database study of vitreoretinal surgery: report 1; case mix, complications, and cataract. Eye (Lond). 2013;27:644–651.
- Wong JG, Sachdev N, Beaumont PE, Chang AA. Visual outcomes following vitrectomy and peeling of epiretinal membrane. Clin Exp Ophthalmol. 2005;33(4):373-378.
- Pournaras CJ, Emarah A, Petropoulos IK. Idiopathic macular epiretinal membrane surgery and ILM peeling: anatomical and functional outcomes. Semin Ophthalmol. 2011; 26(2): 42-46.
- Fraser-Bell S, Guzowski M, Rochtchina E, Wang JJ, Mitchell P. Five-year cumulative incidence and progression of epiretinal membranes: the Blue Mountains Eye Study. Ophthalmology 2003; 110(1): 34-40.
- Tanikawa A, Shimada Y, Horiguchi M. Comparison of visual acuity, metamorphopsia, and aniseikonia in patients with an idiopathic epiretinal membrane. Jpn J Ophthalmol. 2018;62(3):280-285.
- Kim JH, Kim YM, Chung EJ, Lee SY, Koh HJ. Structural and functional predictors of visual outcome of epiretinal membrane surgery. Am J Ophthalmol. 2012;153(1):103-10.e1
- Shimozono M, Oishi A, Hata M, Matsuki T, Ito S, Ishida K, Kurimoto Y. The significance of cone outer segment tips as a prognostic factor in epiretinal membrane surgery. Am J Ophthalmol. 2012;153(4):698-704, 704.e1
- Watanabe K, Tsunoda K, Mizuno Y, Akiyama K, Noda T. Outer retinal morphology and visual function in patients with idiopathic epiretinal membrane. JAMA Ophthalmol. 2013;131(2):172-177.
- Suh MH, Seo JM, Park KH, Yu HG. Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol. 2009;147(3):473-480.e3.
- Massin P, Allouch C, Haouchine B, Metge F, Paques M, Tangui L, Erginay A, Gaudric A. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol. 2000;130(6):732-739.
- Koo HC, Rhim WI, Lee EK. Morphologic and functional association of retinal layers beneath the epiretinal membrane with spectral-domain optical coherence tomography in eyes without photoreceptor abnormality. Graefes Arch Clin Exp Ophthalmol. 2012;250(4):491-498.
- Song SJ, Lee MY, Smiddy WE. Ganglion cell layer thickness and visual improvement after epiretinal membrane surgery. Retina. 2016;36(2):305-310.
- Cho KH, Park SJ, Cho JH, Woo SJ, Park KH. Inner-retinal irregularity index predicts postoperative visual prognosis in idiopathic epiretinal membrane. Am J Ophthalmol. 2016;168: 139-149.
- Govetto A, Lalane 3rd RA, Sarraf D, Figueroa MS, Hubschman JP. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99-113.